The cornea is your eye’s clear, outermost layer, which is critical to focusing your vision. Although transparent, the cornea is actually an intricate, highly organized tissue. Yet, unlike most of your body’s tissues, your cornea doesn’t have blood vessels to protect against infection. The cornea’s nourishment comes from tears and a fluid that lies behind it called “aqueous humor.”
The cornea is your eye’s clear, outermost layer, which is critical to focusing your vision. Although transparent, the cornea is actually an intricate, highly organized tissue. Yet, unlike most of your body’s tissues, your cornea doesn’t have blood vessels to protect against infection. The cornea’s nourishment comes from tears and a fluid that lies behind it called “aqueous humor.”
The cornea is made up of five important layers:
- Epithelium is the cornea’s outermost layer. The epithelium primarily blocks foreign material such as dust, water, and bacteria. Its smooth surface also allows oxygen and nutrients from tears to be absorbed and distributed to the cornea’s inner layers.
- Bowman’s membrane is a thin film of tissue made up of hearty protein fibers, also referred to as collagen. If injured, this layer is at risk of scarring and can lead to vision loss.
- Stroma is the thickest of the cornea’s layers. The stroma layer is composed mainly of water and collagen, which is what maintains its transparency and shape.
- Descemet’s membrane is a thin, yet strong film of tissue made of collagen fibers. Descemet’s membrane protects against injury and infection, and repairs itself easily after injury.
- Endothelium is the cornea’s innermost layer. This layer is responsible for pumping out excess fluid that normally leaks slowly from inside the eye into the stroma. It contains endothelial cells that keep the eye clear.
Why Tears Matter to the Cornea
Whenever you blink, a thin layer of tears covers the cornea to keep your eye moist. It also helps wounds heal and protects against infection. This tear film is made up of three layers, which are important to proper eye health.
- The top lipid layer is made of oil that keeps tears from evaporating too quickly from the eye.
- The middle aqueous layer provides nutrients, elements, and proteins for corneal wound repair and resistance against infection.
- The bottom mucin layer helps spread the aqueous layer across the eye so that it remains wet.
Common Conditions That Affect the Cornea
- Injuries. The cornea usually heals on its own after minor injuries or scratches. A deeper injury can cause corneal scarring which can impair vision and possibly lead to vision loss.
- Allergies can be caused by environmental triggers such as pollen, dust mites, mold, or pet dander, especially if the environment is warm and dry. This is what causes our eyes to itch, burn, turn red, water up, and generally feel irritated.
- Keratitis is an inflammation of the cornea. Infectious keratitis is the most common. This is caused by bacteria, viruses, fungi or parasites in the eye, or wearing contacts with poor hygiene. Noninfectious keratitis can be caused by minor injury or wearing contact lenses too long.
- Dry eye syndrome occurs when your eyes produce fewer or lower quality tears to keep the eye’s surface lubricated. Dry eye symptoms include a scratchy feeling as if something is in your eye, stinging, burning, eye discharge, or pain and redness. Dry Eye Institutes of America™ is a separate clinic within our practice dedicated to the diagnosis and treatment of this common, easily treatable condition.
Corneal Dystrophies
A corneal dystrophy occurs when one or more layer of the cornea lose normal clarity. This is due to a buildup of material that clouds the cornea. Corneal dystrophies are usually inherited, affect both eyes, and progress gradually. Different types of dystrophies include:
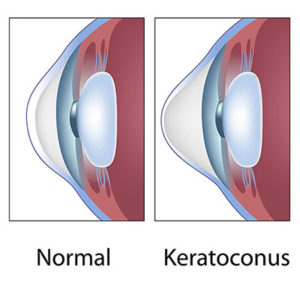
- Keratoconus is caused by a decrease in the protective antioxidants in the cornea, causing the cornea to become thin, bulge outward, and form a rounded cone shape. This can result in blurred vision, nearsightedness, astigmatism and increased sensitivity to light.
- Fuch’s Dystrophy is caused by fluid leaking into the cornea because the endothelial cells have weakened. This can result in corneal swelling and vision loss due to excess fluid leaking into the cornea.
Corneal Cross-Linking (CXL)
This minimally invasive, in-office procedure is also referred to as corneal collagen cross-linking (CXL). It’s designed to strengthen the cornea if it has been weakened, usually by keratoconus.
A healthy cornea has “crosslinks” that connect its collagen fibers, keeping it strong enough to retain its normal shape. Corneal cross-linking increases these crosslinks to help the cornea retain its normal shape and prevent further vision loss.
The CXL procedure applies liquid riboflavin (vitamin B2) to the surface of the eye followed by a controlled ultraviolet light. This is to eliminate corneal ectasia, which is mostly associated with keratoconus. However, corneal ectasia can also relate to irregular astigmatism that can develop after LASIK or PRK. Corneal cross-linking is fully FDA approved and we perform these procedures in our office.
At Eye Consultants of Texas, we treat all varieties of corneal diseases and conditions for patients across the Dallas-Fort Worth Metroplex. Our doctors will carefully diagnose your condition so that you’ll receive exactly the right treatment. Call our office at 817-410-2030 for more information or to schedule an appointment.